Clinics training clinics on how to expand behavioral health care
How Oregon’s Providence Medical Group is helping a PSJH’s Northern California system integrate mental health into primary care
As many as two out of five patients seen in primary care also have behavioral health concerns. And though primary care clinics are where many patients turn to seek mental health consultation and treatment, many U.S. health care providers still struggle to meet their needs.
Dr. Vanessa Casillas, Providence Medical Group’s director of psychology, knows change is possible for Americans suffering from behavioral health problems who think they have nowhere to turn. Over the course of nearly a decade, she’s led Providence Medical Group, in Oregon, on a journey to make behavioral health care as seamlessly available as possible in its primary care clinics.
“A different approach, known as behavioral health integration in primary care, improves access and address a lot of patient’s needs — biological, psychological, social and spiritual — in the context of the medical home in a way that improves coordination of care and helps patients manage their whole health,” she said.
Promoting behavioral health integration in primary care is a top priority for Well Being Trust, which works alongside Providence St. 
Since implementing the behavioral health integration in primary care model, Casillas and her colleagues have seen significant improvements in access to care as well as improved treatments for depression and anxiety.
Now, they are working to share what they have learned by partnering with St. Joseph Medical Group in northern California to provide consultation as they find a place for behavioral health integration in their clinics, too, and aim to meet more patients’ mental health needs.
Finding the right model
Though Providence Medical Group has had measurable success using embedded care, putting it in place involved a great deal of trial-and-error and took years to perfect. From assigning billing codes to determining the best division of work among providers, Casillas and her team had to consider the impact of every decision, learning as they went. All the while, they kept in mind the stigma around mental health and staff’s facility with addressing these concerns so the medical group could make sure patients would feel comfortable seeking and receiving care.
The most challenging — and most important — decision came in the beginning, when they had to decide on the right model of care. Casillas and her team weighed whether a traditional 45- to 60-minute therapy model or a brief, 15- to 30-minute consultation model would best fit the needs of their patient population.
Though the brief consultation model would require Providence to identify other places in the community or along their care continuum where they could refer patients who needed a higher level of care, the traditional therapy model would limit the number of patients that providers would be able to see each day.
Ultimately, Providence opted for the former to reach more patients, Casillas said. And, in the last 12 months, the team has completed 47,000 appointments.
Partnership for success
After all of their efforts, Providence behavioral health leadership team was more than ready to share their years of learnings and help St. Joseph Health Medical Group (SJHMG) integrate behavioral health and primary care in a way that is tailored to the needs of its community. Representing three large areas from wine country to the Oregon border, the northern California system serves a vast region where behavioral health resources are in high demand but low supply.
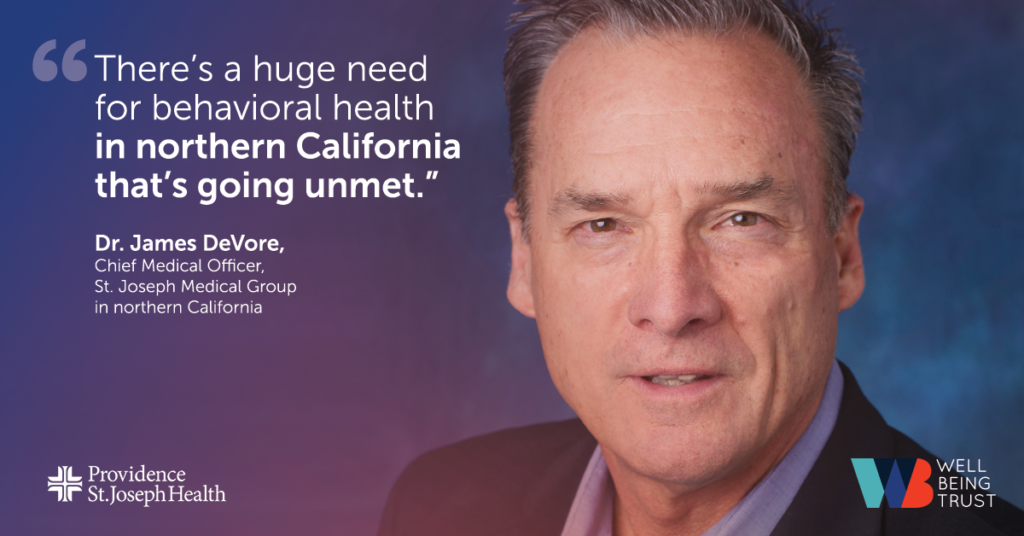
“There’s a huge need for behavioral health care in northern California that’s going unmet,” said Dr. James DeVore, chief medical officer of St. Joseph Health Medical Group (SJHMG). Most patients have to find private behavioral health providers on their own, but that’s tough, he said, because steep housing costs, destruction from wildfires and, in remote Humboldt County, a wet climate deter behavioral health specialists from coming to the area.
Since January, the team at Providence has been guiding DeVore and his northern California SJHMG team as they develop protocols for a new embedded care model and work to recruit providers. So far, St. Joseph has hired a psychiatrist who will serve as a regional resource to the entire behavioral program. The next step is to hire five behavioral health providers — two each for Sonoma and Humboldt Counties, and one for Napa County.
The two medical groups also have been shadowing each other’s clinic staff and meeting to discuss the structure and needs of each of their communities. In the future, Casillas said they hope to help St. Joseph scale and spread their behavioral health work across their entire group.
Those involved say the partnership has benefitted both sides, with providers of both systems sharing resources and knowledge and reaching out to each other for help and guidance.
“In addition to learning from the other region — whether it’s about workflows and assessment tools or integrating behavioral health care — we’re forming valuable relationships with colleagues in California who want to work together,” said Dr. Robin Henderson, chief executive of behavioral health at Providence Medical Group and clinical liaison to Well Being Trust. The ultimate beneficiaries of those relationships, she said, will be both systems’ patients.
“We could not be more appreciative of the support and expertise we have received from Robin and Vanessa and the Oregon team” states Dr DeVore. “Aside from our deeply held dispute about Oregon vs Sonoma pinot noir we have a fantastic relationship!”