Aiming for zero
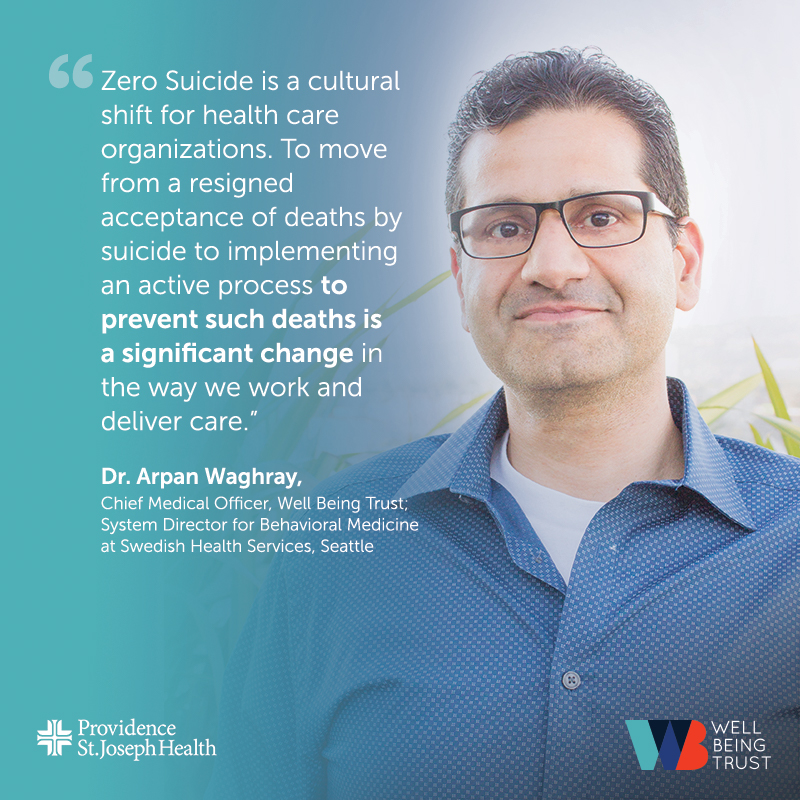
Dr. Arpan Waghray discusses how Well Being Trust is Supporting Providence St. Joseph Health in working to reduce deaths by suicide
Pioneered by the Henry Ford Health System, Zero Suicide develops a systematic process through which caregivers assess and reduce the risk of suicide among their patients. The model gained widespread recognition after Henry Ford experienced an 18-month period with no suicide deaths in 2009-2010.
As Well Being Trust’s Chief Medical Officer, Dr. Arpan Waghray (who is also system director for behavioral medicine at Swedish Health Services, within Providence St. Joseph’s health) is working with a team, including Drs. Robin Henderson, Paul Giger, and Howard Mun to help guide an effort to implement Zero Suicide across a system that spans seven states.
We spoke to Dr. Waghray about why Well Being Trust and Providence is aiming for zero suicides, challenges to the approach, and how the initiative is being rolled out.
Why is the Zero Suicide movement important within the health care industry?
Zero Suicide is a cultural shift for health care organizations. To move from a resigned acceptance of deaths by suicide to implementing an active process to prevent such deaths is a significant change in the way we work and deliver care.
The movement has been taking off for quite some time. Deaths by suicide impact caregivers, patients and family members alike, and people recognize it’s time to do better. Zero Suicide is driven by aspiration, but the rationale and core components of the initiative are based in good science. As we consider how to reliably and consistently provide for patients in crisis, we need to ensure that every place where we offer care is prepared to carry out these new standards.
Where are you in the implementation process?
The first step is to complete a Zero Suicide self-study which helps organizations understand their readiness to implement the initiative. It takes into consideration our current state of care to help create a plan that meets us where we’re at. This includes looking at things like how well we screen for warning signs in our various care centers, what protocols we have in place to ensure evidence-based care for patients in need of a safety plan, and how we provide care in context and connect patients with next levels of care.
Each of our seven regions — Washington, Montana, Oregon, California, Texas, Alaska, and New Mexico — is completing the self-study for their system, as well as for their various service areas in order to identify higher risk areas that may need a different or more specific approach. Once we have completed this process, we will use the information to develop a strategic plan for implementing Zero Suicide across the entire Providence system.
What are the challenges in making such a wide-scale change?
Right now, there’s a lot of variability across service areas and regions. Caregivers in some areas know how to address the subject; others do not. We’re trying to move toward a place where we can provide patients with a high level of reliability and best practices no matter where they are in our system, but we need to be very thoughtful about how we do so.
The goal of Zero Suicide is for there to be no harm done or errors made, but it’s unrealistic to aim that high without what the Zero Suicide movement’s founders call a “just culture.” The expectation of no errors can generate anxiety among caregivers, so we have to be clear that this isn’t about shaming them or putting them under scrutiny over things that may have been out of their control. Rather, it’s about driving a cultural shift and putting processes in place to ensure everyone can do their very best to help patients in moments of despair.
 What else will need to be done for Zero Suicide to be fully effective?
What else will need to be done for Zero Suicide to be fully effective?
Right now, we’re focused on getting ourselves organized around a common cause — ending deaths by suicide — and creating a process to help understand where we are and what we need to do to reach that goal. In the years to come, we will have to figure out how to best allocate resources and measure effectiveness of the initiative’s various interventions.
And, while we want to do the best we can, we can’t prevent deaths by suicide by focusing only on our health system. Another significant part of this process is finding ways to partner with the communities we’re in, such as schools, law enforcement, first responders and faith-based communities.
Ultimately, we don’t need to be constantly reinventing the wheel. There are many groups implementing Zero Suicide, like the Henry Ford Health System. As we move ahead, we look forward to sharing and learning from others along the way.
That said, Well Being Trust hopes our implementation can become a gold standard model for other large health systems that span across multiple regions, so we can advance an integrated approach to suicide prevention—and get to zero—across the country.


 What else will need to be done for Zero Suicide to be fully effective?
What else will need to be done for Zero Suicide to be fully effective?